Dysautonomia
Autonomic Nervous System ANS
- Your Autonomic Nervous System (ANS) is a very important homeostatic control mechanism in your body
- Your ANS helps control many functions
- If your ANS is not functioning properly, this
can lead to many symptoms
- This is known as autonomic dysfunction
The Autonomic Nervous System ANS
- First described by Dr Francis Pottenger in his book “Symptoms of Visceral Disease”, originally published in 1919
Autonomic Nervous System (ANS)
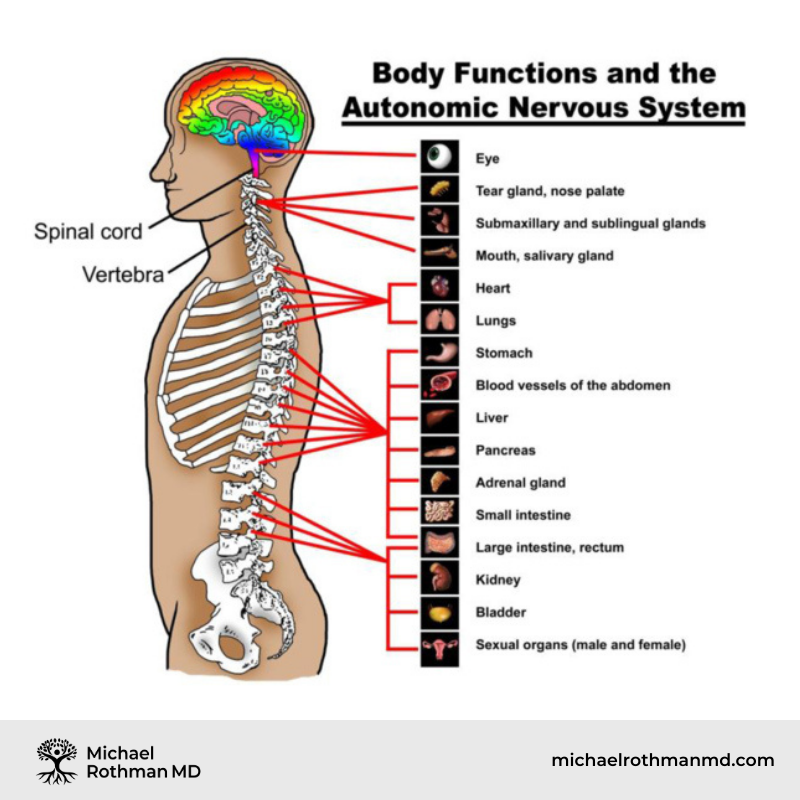
- Your ANS sends signals to all of your organ systems
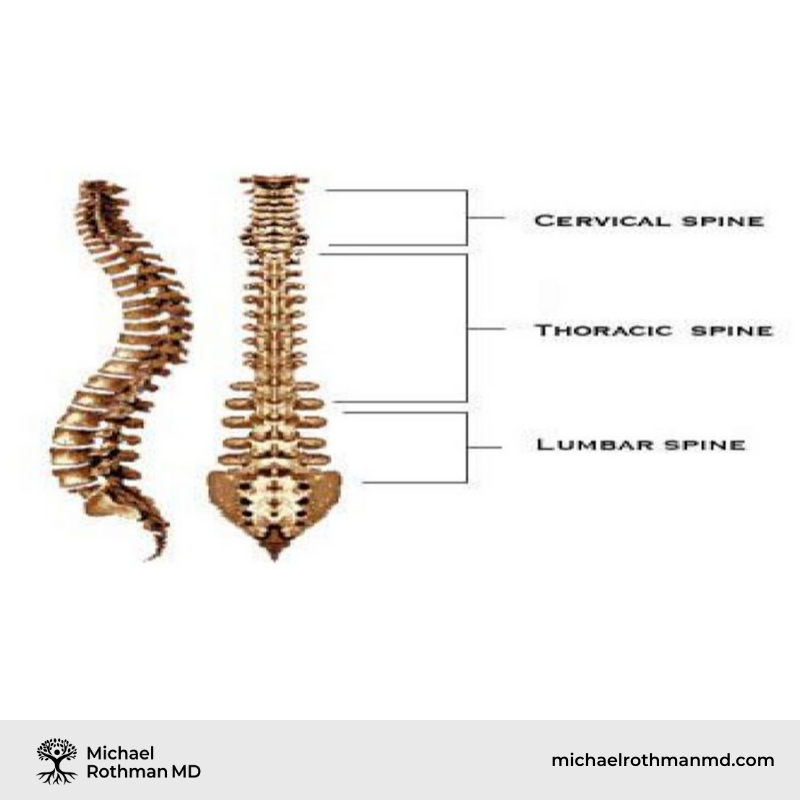
- These signals are sent through nerves which run up and down your spine and then branch off at various levels to innervate your organs
Three Spinal Segments Housing Your ANS
Is Functional Metabolic Testing the
Key to Unlocking Your Wellness?
Your Autonomic System has two Sides
- Sympathetic Nervous System – known as the “fight or flight” response – stimulates vasoconstriction, raises blood pressure and heart rate, slows down gastrointestinal (GI) and urinary system (GU), raises body temperature, many other effects
- Parasympathetic Nervous System – known as the “rest and digest” response – stimulates vasodilatation, lowers blood pressure and heart rate, speeds up gastrointestinal (GI) and urinary system (GU), lowers body temperature, many other effects
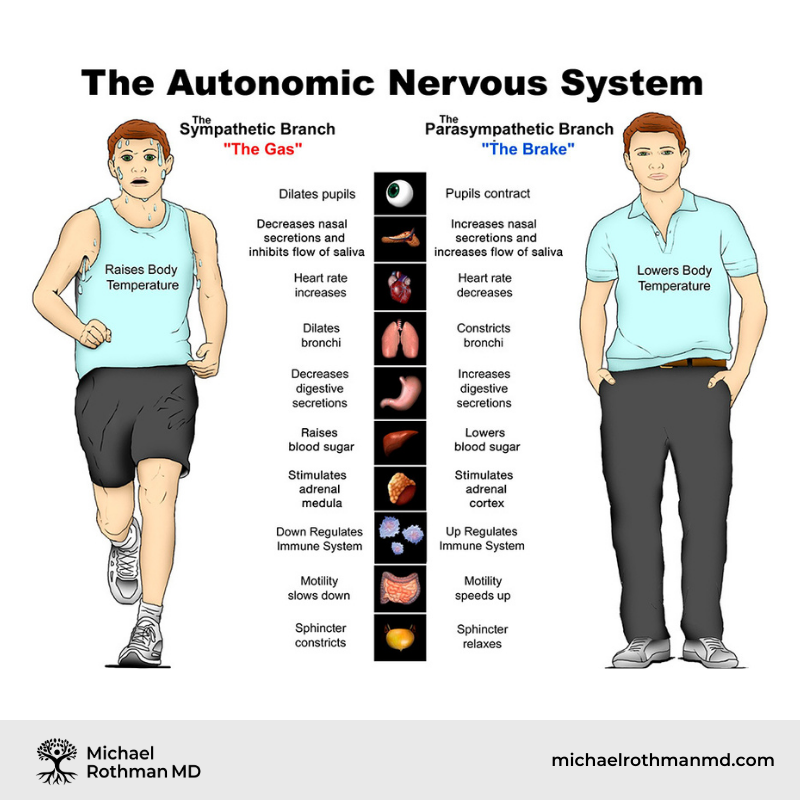
Every Organ System in Your Body is Under Autonomic Control – SNS
- Sympathetic Nervous System (SNS) – Fight or Flight Response – prepare to run or fight for your life. Gastrointestinal system slows down – digestion of food, movement of food stuffs through your GI system, production of stomach acid and digestive enzymes all reduced.
Excess Sympathetic Nervous System (SNS) Activity can Contribute to Many Symptoms
- Vasoconstriction from excess SNS activity decreases blood flow to your brain, and can cause headaches
- Stress headaches, tension headaches – general caused by vasoconstriction
- Hyperthyroidism – increases SNS activity
- Fluctuating blood sugars (Edibolic Stress) can stimulate excess SNS activity
- Frequent symptoms – constipation, thin, ribbon like stools, decreased urge to defecate, reflux
- There may be other symptoms of elevated SNS activity – slow urine flow, urinary retention, anxiety, high blood pressure, tachycardia, dry mouth, dry nose, insomnia, cold hands and feet, excessive sweating, high blood sugar, dry eyes, blurry vision….
Treating Excess SNS Activity
- Vitamins, minerals and amino acids that stimulate PNS can be helpful (Complex S, Taurine )
- Caffeine stimulates SNS (note that certain OTC headache medications contain caffeine) and should be avoided
- Tyramines – can cause vasoconstriction headaches
- Avoid cured and processed meats (hot dogs, bacon) Fermented foods
- (sauerkraut, pickled foods, soy products
- Stabilizing your blood sugar is important – eating enough saturated fat at each meal (“the log on the fire”), reduces autonomic dysfunction
Every Organ System in Your Body is Under Autonomic Control – PNS
- Parasympathetic Nervous System (PNS) – Rest and Digest Response – recover from activity, digest and assimilate ingested food. Gastrointestinal system speeds up – digestion of food, movement of food stuffs through your GI system, production of stomach acid and digestive enzymes all increased.
Excess Parasympathetic Nervous System (PNS) Activity can Contribute to Many Symptoms
- Vasodilatation from excess PNS activity increases blood flow to your brain, and can cause headaches
- Migraines, cluster headaches and exercise headaches – generally caused by vasodilatation
- Estrogen Dominance (too much Estrogen, not enough Progesterone) is a common cause of excess PNS activity and headaches.
- Hypothyroidism – increases PNS activity
- Fluctuating blood sugars (Edibolic Stress) can stimulate excess PNS activity
- Other frequent symptoms of excess PNS- frequent and urgent defecation, increased mucus production, wet stools, increased urge to defecate, excessive gas and bloating, eating stimulates urgent need to defecate.
- There may be other symptoms of elevated PNS activity – frequent and urgent urination and urinary incontinence, depression, low blood pressure, bradycardia, drooling of saliva, watery eyes, post nasal drip, hypoglycemia, asthma, difficulty seeing in the dark….
Treating Excess PNS Activity
- Vitamins, minerals and amino acids that stimulate SNS can be helpful (complex P)
- If Estrogen Dominance is a problem, hormonal therapy is therapeutic (DIM, Calcium-D-Glucarate, Progesterone and testosterone replacement)
- Caffeine stimulates SNS (note that certain OTC headache medications contain caffeine)
- Stabilizing your blood sugar – eating enough saturated fat at each meal (“the log on the fire”), reduces autonomic dysfunction
- Some prescription medications work by causing a vasoconstriction of your blood vessels including Ergot Alkaloids,Triptans and CGRP antagonists
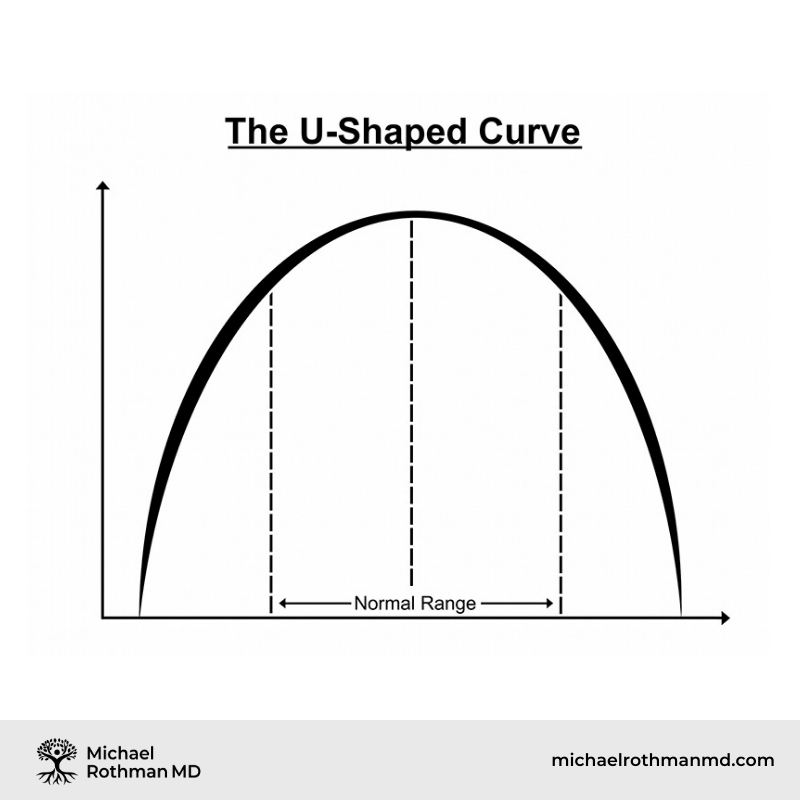
ANS Balance is Achieved Toward the Middle of the Curve
What are the Root Causes of Autonomic Dysfunction?
- What causes autonomic dysfunction in the first place?
- Chronic Stress – many factors – overwork, lack of rest, too much exercise, lack of, or poor quality sleep, EMF exposures, “Stealth Organisms”, environmental exposures…
- Poor diet – fluctuating blood sugar levels
- Hormonal Imbalances
Chronic Stress and Unhealthy Habits Deplete Your Adrenal Reserves and can Contribute to Autonomic Dysfunction

Autonomic Dysfunction can be Ameliorated by Reducing Stressors on your Autonomic Nervous System (ANS)
- Avoid dietary sugar and reduce excess carbs and eat enough healthy (saturated) fats to stabilize your blood sugar reducing ANS stress
- Avoid dangerous environments which then stimulate your flight or flight response (leading to episodes of tachycardia)
- Practice “mind-body” techniques to help reduce limibic dysfunction contibuting to ANS stress
- Practice healthy habits sleep-wake cycles, activity/rest to reduce stressors on your ANS
For Optimal Adrenal Health – Add “Good” Things – Healthy Food, Clean Air, Beneficial EMF’s, Good People increase your Adrenal Reserves and Decrease Autonomic Dysfunction

Ready to Take Control of Your Health?
If you are experiencing symptoms of hormonal imbalances and are seeking effective, metabolically directed treatments, contact us online or call (732) 268-7663 for a consultation.
Unstable Blood Sugar is a Very Common Cause of ANS Dysfunction
- Excessively high blood sugars will stimulate your PNS to release insulin to lower your blood sugar
- Excessively low blood sugars will stimulate your SNS to release adrenaline to raise your blood sugar
- Therefore, Fluctuating blood sugars stress both SNS and PNS
Your Metabolism is Like a Fire
- You “burn” things to create energy
- If you put paper on a fire, the fire will burn up and then burn down very rapidly
- Carbohydrates and sugars are akin to paper on your metabolic fire
- Consequently, meals that consist mostly of carbohydrates and sugars contribute to fluctuating blood sugars and autonomic dysfunction
How Can I Keep my Blood Sugars More Stable?
- Put a “Log on the Fire” every meal • The “Log on the Fire” = Good Fats
- What kind of fat should I consume?
Saturated Fats, Won’t They Hurt Me?
- This is not true
- The notion that saturated fat is bad was created by the food industry to sell margarine, vegetable and seed oils
Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease
- Patty W Siri-Tarino, Qi Sun, Frank B Hu and Ronald M Krauss 1 From the Children’s Hospital Oakland Research Institute Oakland CA Harvard School of Public Health Boston MA.
- ABSTRACT
- Background: A reduction in dietary saturated fat has generally been thought to improve cardiovascular health.
- Objective: The objective of this meta-analysis was to summarize the evidence related to the association of dietary saturated fat with risk of coronary heart disease (CHD), stroke, and cardiovascular disease (CVD; CHD inclusive of stroke) in prospective epidemiologic studies.
- Design: Twenty-one studies identified by searching MEDLINE and EMBASE databases and secondary referencing qualified for inclusion in this study. A random-effects model was used to derive composite relative risk estimates for CHD, stroke, and CVD.
- Results: During 5–23 y of follow-up of 347,747 subjects, 11,006 developed CHD or stroke. Intake of saturated fat was not associated with an increased risk of CHD, stroke, or CVD. The pooled relative risk estimates that compared extreme quantiles of saturated fat intake were 1.07 (95% CI: 0.96, 1.19; P = 0.22) for CHD, 0.81 (95% CI: 0.62, 1.05; P = 0.11) for stroke, and 1.00 (95% CI: 0.89, 1.11; P = 0.95) for CVD. Consideration of age, sex, and study quality did not change the results.
- Conclusions: A meta-analysis of prospective epidemiologic studies showed that there is no significant evidence for concluding that dietary saturated fat is associated with an increased risk of CHD or CVD. More data are needed to elucidate whether CVD risks are likely to be influenced by the specific nutrients used to replace saturated fat.
Harvard Medical School Published in the American Journal of Clinical Nutrition January 2010
- Conclusions: A meta-analysis of prospective epidemiologic studies showed that there is no significant evidence for concluding that dietary saturated fat is associated with an increased risk of CHD or CVD
Problem – Eating a Low Fat Diet
- Myth – eating fat makes you fat
- Fact- Excessive carbohydrates (and even excessive protein) can raise your insulin levels leading to fluctuating blood sugars, autonomic dysfunction, weight gain and many other health problems
- Solution – eat a substantial portion of healthy fats with each meal
Is Breast Milk Good for Babies?
- Of Course breast milk is good for babies
- 55% of the calories from breast milk come from Saturated Fats
- Breast Milk is also contains large quantities of Cholesterol
- Therefore, we must conclude that cholesterol and saturated fats are good for babies
What about Adults?
- Both cholesterol and saturated fat are vital to the health of adults
- In fact, low levels of saturated fats lowers levels of HDL “good cholesterol”
Effect of low-fat diets on plasma high-density lipoprotein concentrations.
- Katan MB.
- Department of Human Nutrition, Wageningen Agricultural University, The Netherlands.
- Low concentrations of HDLs in plasma are a strong predictor of risk for coronary as well as other cardiovascular diseases. There is increasing evidence that this relation is causal and that interventions that change HDL concentrations also change risk. One such intervention is exchanging fat and carbohydrate. In controlled trials, low-fat, high-carbohydrate diets decrease HDL concentrations. The effect is strongest when carbohydrates replace saturated fatty acids, but is also seen when carbohydrates replace mono- and polyunsaturated fatty acids carbohydrates. The effect is seen in both short- and long-term trials and therefore appears to be permanent. This finding is supported by epidemiologic studies in which populations eating low-fat, high-carbohydrate diets were shown to have low HDL concentrations. Weight losses with consumption of low-fat diets could theoretically counter effects on HDL, but in published trials weight losses have been modest and insufficient to offset the decrease in HDL concentrations induced by carbohydrates. Thus, replacement of saturated fat by carbohydrates adversely affects plasma HDL concentrations; replacement of saturated fat by unsaturated fatty acids deserves consideration as an alternative.
- PMID: 9497172 [PubMed – indexed for MEDLINE]
High Carbohydrate Diets, Triglyceride Rich Lipoproteins, and Coronary Heart Disease Risk American Journal of Cardiology 2000
- Abbasi F, McLaughlin T, Lamendola C, Kim HS, Tanaka A, Wang T, Nakajima K, Reaven GM.
- Stanford University School of Medicine, California, USA.
- In this study we compared the effects of variations in dietary fat and carbohydrate (CHO) content on concentrations of triglyceride-rich lipoproteins in 8, healthy, nondiabetic volunteers. The diets contained, as a percentage of total calories, either 60% CHO, 25% fat, and 15% protein, or 40% CHO, 45% fat, and 15% protein. They were consumed in random order for 2 weeks, with a 2-week washout period in between. Measurements were obtained at the end of each dietary period of plasma triglyceride, cholesterol, low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, remnant lipoprotein (RLP) cholesterol, and RLP triglyceride concentrations, both after an overnight fast and throughout an 8-hour period (8 A.M. to 4 P.M.) in response to breakfast and lunch. The 60% CHO diet resulted in higher (mean +/- SEM) fasting plasma triglycerides (206 +/- 50 vs 113 +/- 19 mg/dl, p = 0.03), RLP cholesterol (15 +/- 6 vs 6 +/- 1 mg/dl, p = 0.005), RLP triglyceride (56 +/- 25 vs 16 +/- 3 mg/dl, p = 0.003), and lower HDL cholesterol (39 +/- 3 vs 44 +/- 3 mg/dl, p = 0.003) concentrations, without any change in LDL cholesterol concentration. Furthermore, the changes in plasma triglyceride, RLP cholesterol, and RLP triglyceride persisted throughout the day in response to breakfast and lunch. These results indicate that the effects of lowfat diets on lipoprotein metabolism are not limited to higher fasting plasma triglyceride and lower HDL cholesterol concentrations, but also include a persistent elevation in RLPs. Given the atherogenic potential of these changes in lipoprotein metabolism, it seems appropriate to question the wisdom of recommending that all Americans should replace dietary saturated fat with CHO.
American Journal of Cardiology 2000
- The 60% CHO diet resulted in higher (mean +/- SEM) fasting plasma triglycerides (206 +/- 50 vs 113 +/- 19 mg/dl, p = 0.03), RLP cholesterol (15 +/- 6 vs 6 +/- 1 mg/dl, p = 0.005), RLP triglyceride (56 +/- 25 vs 16 +/- 3 mg/dl, p = 0.003), and lower HDL cholesterol (39 +/- 3 vs 44 +/- 3 mg/dl, p = 0.003) concentrations, without any change in LDL cholesterol concentration
American Journal of Cardiology 2000
- 2 weeks on the lower carbohydrate/higher saturated fat diet cut triglycerides almost in half, while at the same time increasing HDL
Low Fat, High Carbohydrate Diets Raise Triglycerides and Lower HDL (“good cholesterol”)
- Many studies reveal that the ratio to triglycerides to HDL is the most important lipid parameter when assessing cardiovascular risk factors
- A higher saturated fat (which raises HDL) and a relatively low carbohydrate diet (which lowers triglycerides) rapidly improves this ratio
How the edible choices you make each day impact your health.
Subscribe to our email list and receive our FREE download of “The Edibolic Diet” an excerpt from my book, Edibolic Stress, delivered straight to your inbox.
All Sex and Adrenal Cortex Hormones are Made From Cholesterol
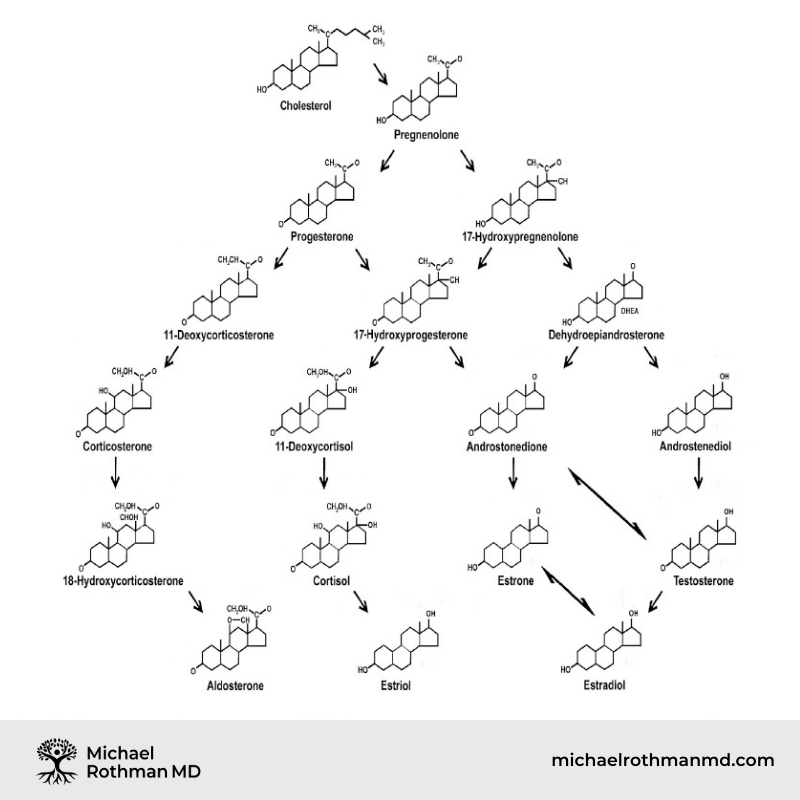
Manifestations of Low Saturated Fat Diet
- Lowers HDL (“good” cholesterol)
- Lowers sex hormone levels
- Contributes to metabolic syndrome (weight gain, high blood pressure, diabetes, heart disease)
- Contributes to development of autonomic dysfunction
Numerous Studies “Proving” That Cholesterol is the Root Cause of Heart Disease were done on Rabbits
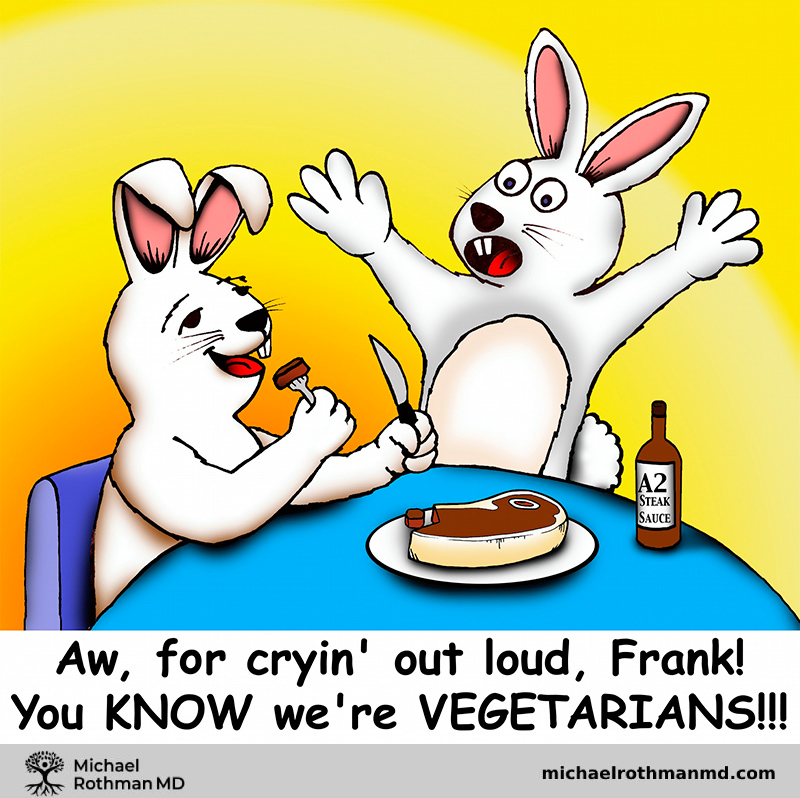
“Everybody knows” there are good fats and bad fats - but the following is really disinformation
- Saturated fats are the “bad” fats
- Unsaturated fats (like fish oil) are the “good” fats
- Saturated fats will clog your arteries
- Saturated fats cause cancer
- Saturated fats are evil and cause every disease know to man…high blood pressure, diabetes, obesity, heart disease
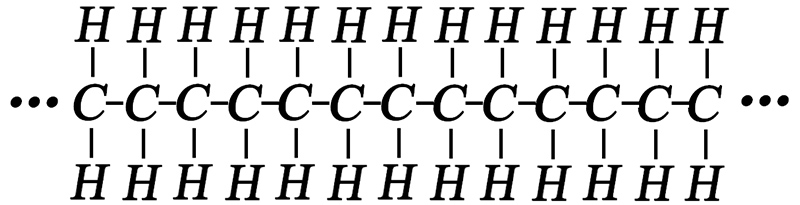
Saturated Fats Have no Double Bonds, They are very Stable and Tend to Stabilize your Blood Sugar
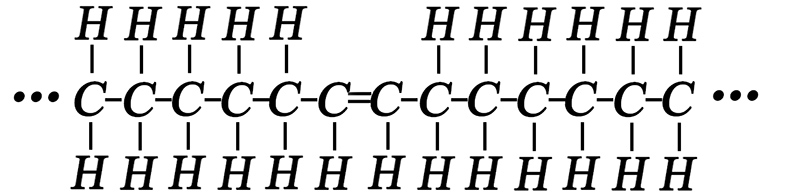
Unsaturated Fats Have Double Bonds – They are unstable and tend to Destabilize your Blood Sugar
To Reduce Autonomic Dysfunction, Put a “Long on the Fire”
- You must eat a sufficient amount of saturated fat at every meal
- These nutrient dense foods will stabilize your blood sugar
- A stable blood sugar improves autonomic nervous system functioning
- These healthy fats also provide building blocks for adrenal cortex and sex hormones
Autonomic Dysfunction Treatment Summary
- Put a “log on the fire” to stabilize blood sugars
- Identify and treat:
- Environmental Issues
- Stealth Organisms
- Thyroid Problems
- Sex hormone Problems
- Other metabolic imbalances
- Other toxins
- Use appropriate nutraceuticals to modulate ANS tone
Subscribe For Expert Insights

