What is intermittent fasting?
- Intermittent fasting is way of timing your meals to allow you to be in a non-fed state for relatively long periods of time.
What is a “non-fed” state?
- A non-fed state also known as the “post-absorptive state” is a physiologic state where your body has consumed easily accessible energy sources like sugar and glycogen. When you have depleted those stores, your body will start using fat as an energy source. You will need to abstain from eating for at least 8-12 before you actually reach the “non-fed” state
- What is the advantage of being in the “non-fed” state?
- While in the “non-fed” state, you will burn your own fat for energy; this will help you to reduce your body fat. More importantly, fasting (being in the non-fed state for extended periods of time) will reduce your insulin levels. Chronically elevated insulin levels (resulting from lack of being in the non-fed state) leads to insulin resistance (IR).
Why is Insulin Resistance (IR) so detrimental to health?
- Research is demonstrating that insulin resistance (IR) is the root cause of many chronic diseases including heart disease, high blood pressure and type II diabetes. IR also contributes to weight gain, hypothyroidism, cancer, mortality from covid-19 and other chronic inflammatory diseases.
Doesn’t a calorie-restricted diet do the same thing?
- No! Calorie restricted diet eventually will fail because your metabolism slows down under conditions calorie restriction. Intermittent fasting dose not restrict caloric intake, instead IF restricts the timing of your meals. IF does not slow your metabolism. Improving your insulin sensitivity will actually increase your metabolism.
Transitioning to Intermittent Fasting
- Step 1 – stop snacking – eat three meals each day – do not eat between meals
- Step 2 – stop consuming sugar, reduce excess carbohydrate intake
- Step 3- Do not eat your first food of the day (breakfast) until you are hungry
- Step 4 – Eat your breakfast later and later in the morning as you start to become more fat adapted
- Step 5 – Eat two meals each day
- Step 6 – eat your first meal later and your last meal earlier to increase the amount of time that you are in the non-fed state
Tips for success
- Reduce your carbohydrate intake levels – carbohydrates stimulate insulin
- Avoid excess amounts of protein – protein can be turned into carbohydrates, which then increase insulin
- Eat healthy fats – Meat, eggs, cheese, coconuts, chicken, pork ….Avoid polyunsaturated fats (PUFA) – PUFA are found in nuts and seeds, nut butters margarine, commercial mayonnaise and salad dressings (usually in the form of canola oil or soy oil) and many processed foods
- Eat real food- avoid protein powders, power bars, avoid processed foods. Protein powders often contain BCAA (branched chain amino acids) that can spike your insulin levels
- Drink plenty of water – avoid juice, diet drinks
- Avoid artificial sweeteners- they can spike you insulin levels
- Get enough restorative sleep – poor sleep is very stressful, raising your cortisol levels, leading to high blood sugar, elevated insulin and finally insulin resistance
- Reduce your stress – any aspect of your life that contributes to excess stress can raise your cortisol levels, leading to high blood sugar, elevated insulin and finally insulin resistance
- Do short bursts of high intensity training (HIT). HIT will help to increase your metabolic rate
- Do not try to starve yourself – this is not sustainable and will slow your metabolism
- Do not overeat when breaking your fast – eat slowly in a calm, relaxed atmosphere.
- Be flexible with your eating schedule
- Plan ahead with what you are going to eat to break your fast-Do not just “grab something” because you are tired or hungry or time pressured
Start your journey to true well-being:
Subscribe to our email list and receive valuable health tips, essential wellness recommendations, and our free guide, “13 Ways to Increase Your Healthspan,” delivered straight to your inbox. Join our community and take the first step towards a healthier tomorrow!
What Should I Eat?
- Put a “Log on the Fire” every meal
- The “Log on the Fire” = Good Fats
- What kind of fat should I consume?
Saturated Fats, Won’t They Hurt Me?
- This is not true
- The notion that saturated fat is bad was created by the food industry to sell margarine, vegetable and seed oils
Numerous Studies “Proving” That Cholesterol is the Root Cause of Heart Disease were done on Rabbits
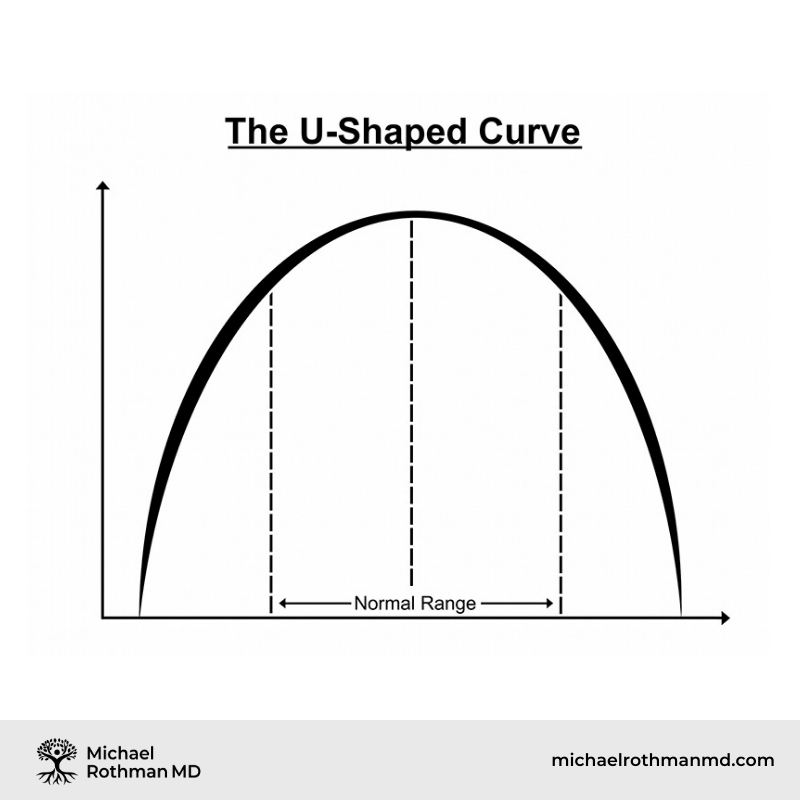
Health is Achieved Toward the Middle of the Curve
Paracelsus
- This is not true
- The notion that saturated fat is bad was created by the food industry to sell margarine, vegetable and seed oils
Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease
- Patty W Siri-Tarino, Qi Sun, Frank B Hu and Ronald M Krauss 1 From the Children’s Hospital Oakland Research Institute Oakland CA Harvard School of Public Health Boston MA.
- ABSTRACT
- Background: A reduction in dietary saturated fat has generally been thought to improve cardiovascular health.
- Objective: The objective of this meta-analysis was to summarize the evidence related to the association of dietary saturated fat with risk of coronary heart disease (CHD), stroke, and cardiovascular disease (CVD; CHD inclusive of stroke) in prospective epidemiologic studies.
- Design: Twenty-one studies identified by searching MEDLINE and EMBASE databases and secondary referencing qualified for inclusion in this study. A random-effects model was used to derive composite relative risk estimates for CHD, stroke, and CVD.
- Results: During 5–23 y of follow-up of 347,747 subjects, 11,006 developed CHD or stroke. Intake of saturated fat was not associated with an increased risk of CHD, stroke, or CVD. The pooled relative risk estimates that compared extreme quantiles of saturated fat intake were 1.07 (95% CI: 0.96, 1.19; P = 0.22) for CHD, 0.81 (95% CI: 0.62, 1.05; P = 0.11) for stroke, and 1.00 (95% CI: 0.89, 1.11; P = 0.95) for CVD. Consideration of age, sex, and study quality did not change the results.
- Conclusions: A meta-analysis of prospective epidemiologic studies showed that there is no significant evidence for concluding that dietary saturated fat is associated with an increased risk of CHD or CVD. More data are needed to elucidate whether CVD risks are likely to be influenced by the specific nutrients used to replace saturated fat.
Harvard Medical School Published in the American Journal of Clinical Nutrition January 2010
- Conclusions: A meta-analysis of prospective epidemiologic studies showed that there is no significant evidence for concluding that dietary saturated fat is associated with an increased risk of CHD or CVD
Breast Milk
- 55% of the calories from breast milk come from Saturated Fats
- Also high in Cholesterol
Low Intake of Saturated Fat
- Lowers Levels of HDL “good cholesterol”
Effect of low-fat diets on plasma high-density lipoprotein concentrations.
- Katan MB.
- Department of Human Nutrition, Wageningen Agricultural University, The Netherlands.
- Low concentrations of HDLs in plasma are a strong predictor of risk for coronary as well as other cardiovascular diseases. There is increasing evidence that this relation is causal and that interventions that change HDL concentrations also change risk. One such intervention is exchanging fat and carbohydrate. In controlled trials, low-fat, high-carbohydrate diets decrease HDL concentrations. The effect is strongest when carbohydrates replace saturated fatty acids, but is also seen when carbohydrates replace mono- and polyunsaturated fatty acids carbohydrates. The effect is seen in both short- and long-term trials and therefore appears to be permanent. This finding is supported by epidemiologic studies in which populations eating low-fat, high-carbohydrate diets were shown to have low HDL concentrations. Weight losses with consumption of low-fat diets could theoretically counter effects on HDL, but in published trials weight losses have been modest and insufficient to offset the decrease in HDL concentrations induced by carbohydrates. Thus, replacement of saturated fat by carbohydrates adversely affects plasma HDL concentrations; replacement of saturated fat by unsaturated fatty acids deserves consideration as an alternative.
- PMID: 9497172 [PubMed – indexed for MEDLINE]
American Journal of Clinical Nutrition
- In controlled trials, low-fat, high-carbohydrate diets decrease HDL concentrations. The effect is strongest when carbohydrates replace saturated fatty acids
Metabolic Syndrome
- A syndrome of high blood pressure, diabetes, obesity and heart disease initially recognized by Dr Reavens
- One of the most important causes of disease in the world
Hippocrates 2,500 Years Ago
- “All Disease begins in the Gut”
- Every time you eat or drink, you are either enhancing your health or promoting disease
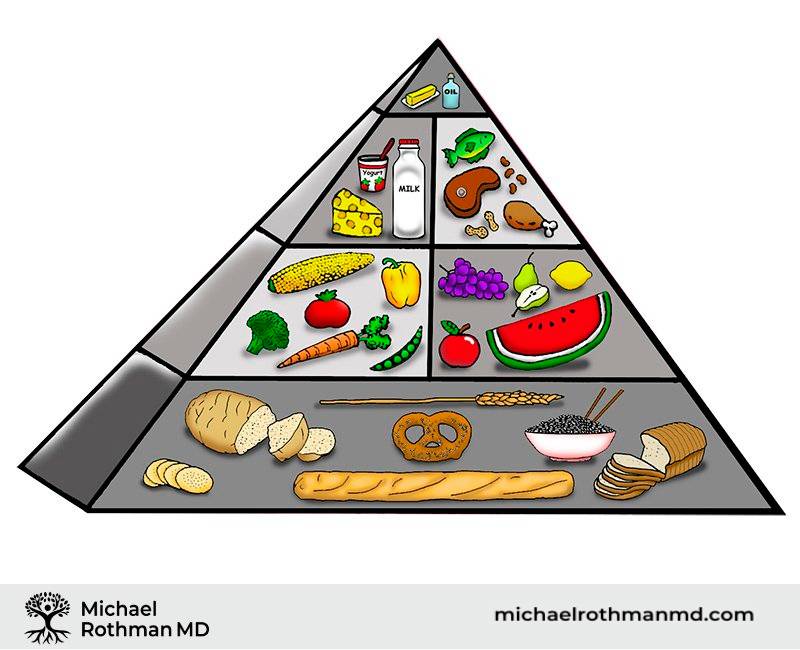
The Food Pyramid, Which is Based on a High Carb-Low Fat Diet Contributes to High Blood Pressure, Diabetes, Obesity and Heart Disease
Hidden or “stealth organisms” – viruses, bacteria, parasites can contribute to chronic stress and adrenal stress
Problem – Eating too Frequently
- Myth – eating small, frequent meals will “boost your metabolism”
- Fact – every time you eat, your pancreas secretes insulin and excess insulin is a root cause of weight gain
- Solution – Eat no more than 3 times each day, no snacking
Ready to Take Control of Your Health?
If you’re ready to prioritize your health and are seeking effective, metabolically directed treatments, contact us online or call (732) 268-7663 for a consultation with Dr. Rothman.
Problem – Eating a Low Fat Diet
- Myth – eating fat makes you fat
- Fact- Excessive carbohydrates (and even excessive protein) can raise your insulin levels leading to weight gain
- Solution – eat a substantial portion of healthy fats with each meal
High Carbohydrate Diets, Triglyceride Rich Lipoproteins, and Coronary Heart Disease Risk American Journal of Cardiology 2000
- Abbasi F, McLaughlin T, Lamendola C, Kim HS, Tanaka A, Wang T, Nakajima K, Reaven GM.
- Stanford University School of Medicine, California, USA.
- In this study we compared the effects of variations in dietary fat and carbohydrate (CHO) content on concentrations of triglyceride-rich lipoproteins in 8, healthy, nondiabetic volunteers. The diets contained, as a percentage of total calories, either 60% CHO, 25% fat, and 15% protein, or 40% CHO, 45% fat, and 15% protein. They were consumed in random order for 2 weeks, with a 2-week washout period in between. Measurements were obtained at the end of each dietary period of plasma triglyceride, cholesterol, low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, remnant lipoprotein (RLP) cholesterol, and RLP triglyceride concentrations, both after an overnight fast and throughout an 8-hour period (8 A.M. to 4 P.M.) in response to breakfast and lunch. The 60% CHO diet resulted in higher (mean +/- SEM) fasting plasma triglycerides (206 +/- 50 vs 113 +/- 19 mg/dl, p = 0.03), RLP cholesterol (15 +/- 6 vs 6 +/- 1 mg/dl, p = 0.005), RLP triglyceride (56 +/- 25 vs 16 +/- 3 mg/dl, p = 0.003), and lower HDL cholesterol (39 +/- 3 vs 44 +/- 3 mg/dl, p = 0.003) concentrations, without any change in LDL cholesterol concentration. Furthermore, the changes in plasma triglyceride, RLP cholesterol, and RLP triglyceride persisted throughout the day in response to breakfast and lunch. These results indicate that the effects of lowfat diets on lipoprotein metabolism are not limited to higher fasting plasma triglyceride and lower HDL cholesterol concentrations, but also include a persistent elevation in RLPs. Given the atherogenic potential of these changes in lipoprotein metabolism, it seems appropriate to question the wisdom of recommending that all Americans should replace dietary saturated fat with CHO.
American Journal of Cardiology 2000
- The 60% CHO diet resulted in higher (mean +/- SEM) fasting plasma triglycerides (206 +/- 50 vs 113 +/- 19 mg/dl, p = 0.03), RLP cholesterol (15 +/- 6 vs 6 +/- 1 mg/dl, p = 0.005), RLP triglyceride (56 +/- 25 vs 16 +/- 3 mg/dl, p = 0.003), and lower HDL cholesterol (39 +/- 3 vs 44 +/- 3 mg/dl, p = 0.003) concentrations, without any change in LDL cholesterol concentration
- 2 weeks on the lower carbohydrate/higher saturated fat diet cut triglycerides almost in half, while at the same time increasing HDL
Manifestations of Low Saturated Fat Diet
- Lowers HDL (“good” cholesterol)
- Lowers sex hormone levels
- Contributes to metabolic syndrome (weight gain, high blood pressure, diabetes, heart disease)
Benefits of Proper Intermittent Fasting
- Sustainable Weight Loss
- Improvement in lipid parameters, lowers triglycerides, raises HDL
- Lowers insulin levels, reduces insulin resistance
- Helps overall health with less inflammation and less chronic degenerative illness